Wednesday Feb 25, 2026
Wednesday Feb 25, 2026
Tuesday, 8 December 2020 02:14 - - {{hitsCtrl.values.hits}}

The stigma associated with COVID-19 and the fear of being cremated is now forcing some sectors of the community to avoid PCR/antigen testing. This could lead to uncontrolled eruption of new clusters – Pic by Shehan Gunasekara
In the last few months, considerable scientific evidence has been published in international peer reviewed journals about the novel coronavirus and its environmental impact, enabling us to remove the veil of ‘unknowns’ and move towards making informed decisions.
Viruses and virology is the domain of microbiologists, more specifically virologists. While these are not my area of expertise either, some basic knowledge in biology can help us understand the present pandemic. It can also help us understand the various precautionary measures that have been put in place, enabling us to follow and appreciate them better. The official name of the virus is SARS-CoV-2 and the disease it causes is called COVID-19.
The decision to make cremation the mandatory form of disposing the COVID-19 dead was based on the premise that there was (i) insufficient evidence on the possibility of the virus leaking out of the buried bodies from the cemeteries, (ii) the possibility of the virus entering the water table, and (iii) as a consequent to (ii), transmission of the virus among the population. The cremation decision was based on precautionary principles, as the SARS-CoV-2 is a new virus with many unknowns.
The virus
A single virus particle (called a virion) consists of an outer shell made of protein, enclosing and protecting the DNA or RNA, the genome or in layman terms the software that runs the virus. It is very tiny (20 to 400 nanometres) and cannot be seen through a microscope. The genome is like an instruction manual for our cells and the entire body to function. Once the virus enters our living cells (called infection), it stops the normal function of a cell and hijacks the cell machinery to produce more copies of the virus, causing the cell to eventually burst open, infecting new cells with virus particles and initiating a chain reaction. Thus, living cells are necessary for the virus to survive and make copies. Other than making more copies of itself, within a live host cell, it has no other function.
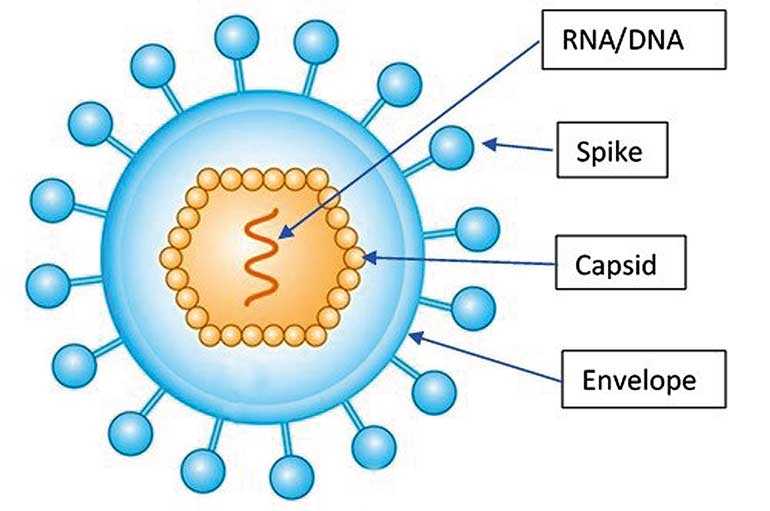
Viruses are broadly divided into Enveloped and Non-Enveloped viruses. The envelope is an outer covering on the virus composed of a fatty substance (lipids) and proteins (see figure). The SARS-CoV-2 virus is an enveloped virus.
Schematic diagram of an enveloped virus
The coronavirus that you see illustrated has knob like spikes on the surface embedded in the lipid envelope. These spikes are vital for the virus to gain entry into our cells in the throat and lungs (respiratory tract): imagine this as the key (spikes) to open the door (cells in the throat and lungs). Fortunately, this envelope provides a soft target and is easily broken down by soap, detergents and other disinfectants such as alcohol. Without this envelope the virus cannot infect us – it has no key to enter our cells. Hence the emphasis on washing our hands with soap and disinfecting the environment with alcohol and detergents – this is sufficient to destroy the virus.
The Non-Enveloped viruses do not have this lipid layer. They have a hard protein coat resistant to common disinfectants, enabling the virus to survive in the outside environment. Examples are the Poliovirus and the viruses causing dysentery.
Stability of the virus in the environment
In the past few months, scientists all over the world have looked at the potential risks of the SARS-CoV-2 virus entering wastewater and serving as a source of infection. Untreated waste (particularly from hospitals) and surface waters are a potential source of disease transmission and research done in these areas are at the initial stages. The virus is shed from patients who are under treatment in hospitals or quarantined at home, through their daily ablutions, sputum, and vomit, which can enter wastewater. Besides, faeces and urine from infected patients are also sources for the virus to enter sewage channels and seep into the water table. How stable are they in the outside environment?
A study on the stability of the virus on different surfaces under different environmental conditions simulated in a laboratory was done by the School of Public Health, Faculty of Medicine, Hong Kong and published in a leading medical journal, the Lancet Microbe (Chin et al. 2020). The major outcomes of this study were:
Temperature: The virus is highly stable at 4 °C (e.g. in the fridge) but sensitive to heat. When the incubation temperature is increased to 70 °C, the virus is inactivated in five minutes. At 22 °C virus is not detected after 14 days and at 37 °C it is not detected after two days. The last two are feasible temperatures in Sri Lanka.
Stability on surfaces: Infectious virus could not be recovered from printing or tissue paper after three hours, from wood or cloth after two days. The virus is more stable on smooth surfaces. Infectious virus could not be recovered from day four from glass and banknotes, and from steel after seven days.
Disinfectants: The virus did not survive common disinfectants such as household bleach, ethanol, etc. It survived soap for five minutes. It also tolerates a pH range of 3 to 10. i.e., it cannot tolerate very low (acidic) or high (very basic) pH. The RNA of the coronaviruses, in general, is extremely fragile and can be rapidly degraded by enzymes (called RNAses) abundant in the natural environment (Brisebois et al. 2018).
Can the virus leak into the environment?
Theoretically virus particles can enter the soil environment after burial of a COVID-19 victim if the corpse is not isolated in the grave by a ‘leak proof’ plastic body bag, as decay and decomposition sets in gradually. However, what enters the soil environment is not an intact virus capable of causing an infection. Once the patient dies, the virus in the body cells cannot multiply and they begin to disintegrate. Viruses need living cells within which they can multiply.
We should remember that the virus is not an active living organism capable of defending itself and transferring to a new host. The decomposing body releases a range of chemicals and enzymes that would breakdown the virus. Other micro-organisms, either from the decomposing body or living in the soil environment, would consume these virus particles. Thus, they have a short survival time in the outside environment where detergents and other chemicals in the wastewater and enzymes produced by bacteria can damage the virus envelope (WHO 2020).
Consider the many patients who have died in the past from very infectious bacterial (Pneumonia, Tuberculosis, Typhoid, Cholera) and viral (Polio, HIV, Ebola) diseases. Cremation was never mandatory for these patients and there has never been any outbreak of epidemics attributed to cemeteries where these patients were buried. Disease causing pathogens are very specialised micro-organisms that can survive only in their living hosts. Once they leave their host and enter the natural environment, they cannot compete with the free-living microorganisms.
A study conducted in Milan, Italy, one of the worst affected regions by the pandemic, to determine the presence of the SARS-CoV-2 virus in wastewaters and rivers, detected RNA of the virus in the untreated wastewaters but not in the treated wastewaters (Rimoldi et al. 2020. However, the virus detected was not infectious, indicating the natural decline of viral pathogenicity. Still, authors suggest adopting a precautionary approach due to the risks for public health.
The question of the water table
The water table is a huge body of water below the surface of the soil. You can find this out by looking into the nearest well. In low lying areas, such as in Colombo, the water table is close to the soil surface particularly during the rainy season. In the up-country regions or the dry regions, the water would be several metres deep in the well.
What is the risk of the virus entering the water table and infecting us? First, chances of finding a complete virus particle capable of causing infection are very small, due to reasons given above. Second, those living in urban area do not consume ground water directly. The water we consume is disinfected at the Water Treatment plants of the Water Board and we also boil the water at home. The WHO has indicated that the virus survives only two days in dechlorinated tap water and in hospital wastewater at 20 ºC, and that there is no evidence that coronaviruses have caused infections through drinking water (WHO 2020).
Thirdly, drinking water is not a source of infection: the virus has to enter through our mouth, nose or eyes to enter the cells in our throat and lungs (respiratory tract), which is the main point of entry. Thus, infection of humans by the corona virus found in the water table is very unlikely.
Transmitting the virus among population
The virus can reach the population, if at all, not only from the ground water but also from the contamination of the environment. This has been addressed by many research studies published in peer-reviewed science journals. The environment is being continuously contaminated from hospitals treating COVID-19 patients and also possibly from those under quarantine at home or quarantine centres (as mentioned earlier).
Detection of the virus in faecal samples has been shown in many studies done using the RT-PCR, the accepted gold standard for detection of viral RNA. However, most if not all, of these studies have cautioned that positive samples may only have the RNA fragment that is amplified by the PCR. A positive PCR does not necessarily mean the detection of infective viable virus; this can only be established by cell cultures of the suspected virus.
A most recent study from Ecuador found positive PCR detection of the SARS-CoV-2 in river water contaminated by untreated sewage (Guerrero-Latorre et al. 2020). The authors caution that what was detected was RNA fragments, which alone cannot transmit the disease.
Corpse handling during COVID-19
Few peer reviewed papers have been published on handling and disposal of corpses of people who died from COVID-19. A publication by Nanayakkara et al. in October 2020 reviews practices worldwide and also the risk of infection after burial from bacterial and viral diseases.
They conclude that due to inadequate knowledge available of COVID-19, it would be prudent to follow the safe corpse handling guidelines recommended by the WHO, until research is conducted on the survival of live viruses in dead bodies. They also state that because virus multiplication ceases as there is no living host, the virus can only spread to other humans by touching the corpse as COVID-19 is a respiratory virus spread mostly by respiratory secretions.
The publication refers to WHO guidelines (WHO 2020), which states that graveyards of those who died from highly infectious diseases should be at least 30 metres from groundwater sources used for drinking water, and grave floors must be at least 1.5 metres above the water table, with 0.7 metre unsaturated zone and that surface waters from graveyards must not enter inhabited zones. Similar guidelines are also available from the Centres for Disease Prevention and Control of the USA (CDC 2020).
Rajanikanta et al. 2020, in an Indian perspective on handling the dead, emphasise the importance of handling the dead with dignity for the deceased and the surviving family. They also underline that more precautions need to be taken to prevent spread of the virus during handling the bodies, as SARS-CoV-19 is a new virus whose virulence and period of survival in the dead body is not yet entirely known. They suggest prevention of infection can be done by disinfection of the dead body with chlorine-based solution, enclosing it in a puncture proof body bag, minimal contact with the body and using airtight boxes for cremation or burial.
A recent article in the British Medical Journal Global Health, where the authors reviewed the available literature to scope and assess the effects of specific strategies for the management of bodies of COVID-19 victims, stated, “There is scarce evidence on the transmission of coronavirus disease 2019 (COVID-19) and other coronaviruses from the dead bodies of confirmed or suspected cases” (Yaacoub et al. 2020).
So, what does the science tell us?
A protocol for safe burial
By taking the above into account, a safe burial protocol is suggested to prevent the virus particles, capable of causing infection, from entering the environment.
The stigma associated with COVID-19 and the fear of being cremated is now forcing some sectors of the community to avoid PCR/antigen testing. This could lead to uncontrolled eruption of new clusters. The cremation of Muslin deceased persons from COVID-19 has polarised and created resentment within the community. As this article shows, the science is out there, as is the evidence, to show that safe burial can be accommodated for this epidemic.
(The writer does research in the Plant and Environmental Sciences. He can be contacted on [email protected])