Thursday Feb 19, 2026
Thursday Feb 19, 2026
Tuesday, 18 May 2021 00:00 - - {{hitsCtrl.values.hits}}
|
Although our understanding of how SARS-CoV-2 spreads continues to evolve, the basic public health interventions that have been recommended since the beginning remain a cornerstone in battling this pandemic: physical distancing, wearings masks, adequate ventilation, avoiding crowded indoor spaces, and sanitising hands – Pic by Shehan Gunasekara
|
Sri Lanka, similar to many other countries in the region, is facing a rapid surge in the number of COVID-19 cases. On 9 May, Sri Lanka recorded 2,672 cases, the highest number of daily cases recorded thus far in the island. Regionally, India, Nepal, Pakistan are all facing challenges ahead with similar trends of cases rising.
One of the reasons for the rise in the number of COVID-19 cases is the emergence of variants. During the last two weeks, B.1.1.7 and B.1.617 variants that were first detected in the UK and India, respectively, were detected in Sri Lanka.
This article will focus on the science behind the COVID-19 variants, helping you understand the scientific process behind variant emergence, the severity of the threat, the impact they have on your health, and common misconceptions. By becoming more informed, we can have a clearer understanding of why each of us needs to help minimise the spread of the virus via public health measures, get vaccinated, and limit the potential of the virus to replicate and create more variants.
So, let’s dive in and equip ourselves with some useful information on variants and fight this virus together.
What are variants?
Viral mutation is a natural process that occurs when an RNA or DNA virus replicates. When a specific set of mutations is selected through multiple rounds of replication, a new ‘variant’ emerges1. There are likely hundreds of SARS-CoV-2 variants – viruses that have a nucleic acid sequence that is slightly different from the virus originally identified in January 2020 (Wuhan-Hu1) — currently circulating worldwide2. Variants are selected and become more common over time because they have an advantage over the original virus—advantages such as being more transmissible or being better at evading a person’s immune response3. Essentially, the virus evolves via mutation as it produces more copies of itself, and the ones that are better at surviving become more prominent.
 Why are there so many names for variants?
Why are there so many names for variants?
It’s fair to say that we have been confused by the various names given to multiple SARS-CoV-2 variants. The bad news is that a consensus has not yet been reached regarding one system4. For example, for the virus commonly refered to as the ‘UK variant,’ the name B.1.1.7 refers to the genetic lineage of the variant and its evolutionary relationship to the original virus. For this same variant, the name 501Y.V1 refers to an amino acid substitution in its spike protein, while the name VOC 202012/01 stands for ‘variant of concern’and includes the month and year of discovery.
The good news is that we know what not to do – which is to not name variants based on the geographic areas where they were first detected. There is a strong consensus within the scientific community and in journalistic ethical standards to avoid using geographic names, which indicate the location where the variant was first detected, when identifying variants5. First, it is impossible to establish when and where a variant first emerges, and since variants rapidly disemminate across the globe, geographic names are technically inaccurate. Second, use of geographic names often adds undue stigma to the locations associated with them. For example, calling a variant the UK or the Indian variant is inaccurate, stigmatising, and can lead to confusion as more variants emerge. The standard is to use names such as B.1.17. As an example, we would not be comfortable if we have to face stigma due to the term ‘Sri Lankan COVID-19 variant.’
Why are we so worried about the variants?
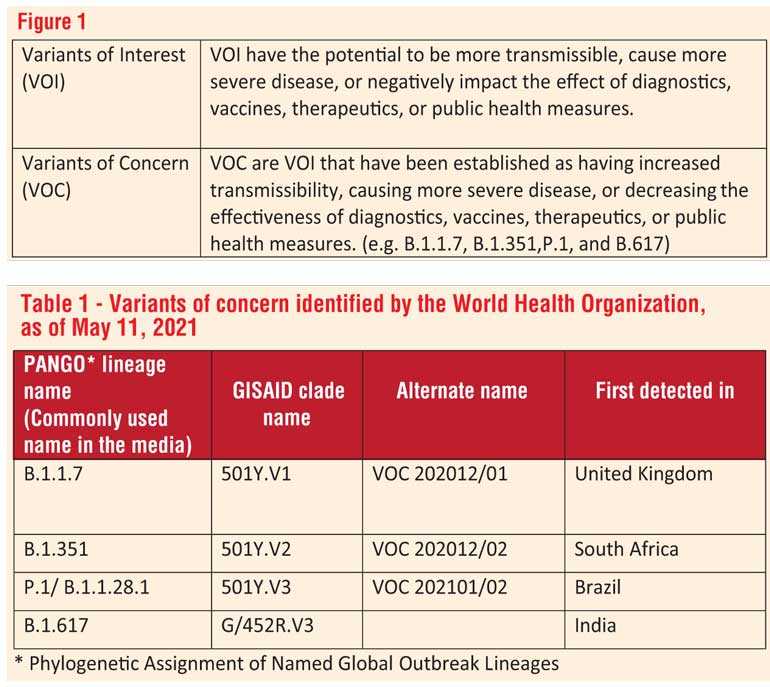
The emergence of variants makes it more difficult for us to gain control over the pandemic. Some variants may be more transmissible than the original virus or cause more severe disease. Even more ominous, variants may render the valuable diagnostic tests, vaccines, and therapeutics that have been developed over the past year less effective. The World Health Organization (WHO) classifies variants as variants of interest (VOI) or variants of concern (VOC) based on their impact on global public health6. And the definitions of the VOI and VOC are straightforward, as outlined in Figure 1.
Over the past few months, three variants have persisted and been named as VOC – B.1.1.7, B.1.351, and P.1, which were first detected in the UK, South Africa, and Brazil, respectively (Table 1). In the past few days, B.1.617, which has been detected in increasing frequency amidst the resurgence of cases in India, has joined the VOC list7. The four VOC all possess over a dozen mutations in the SARS-CoV-2 genome, including multiple mutations in the gene sequence for the spike protein, which is used by the virus to bind to and enter cells.
For easier reference, Table 1 summarises the variants of concern, the technical names and the regions in which they were first detected.
It is crucial to note that terms such as ‘double mutant’ and ‘triple mutant’ are incorrect, since these variants all possess multiple mutations8. The ‘double mutant’ terminology arose because mutations in B.1.617 were also found in other VOC. The ‘triple mutant’ terminology arose because an additional mutation was found in the spike protein, and this variant may have the potential to increase transmissibility or severity.
The rise of variants emphasises the need to expand capacity for sequencing technology, since we can only detect new variants by sequencing the genome of the virus. Public genomic repositories such as Nextstrain and GISAID, which allow sharing of viral genomic data within the global scientific community, are critical for tracking and tackling the pandemic on a global scale9, 10.
How do the VOC affect our existing diagnostics, therapeutics, and vaccines?
Diagnostic tests detect the virus’ genetic sequence (RNA), proteins on the virus (antigens), or the person’s immune response to SARS-CoV-2 (antibodies). Many of the existing SARS-CoV-2 tests were developed using the original nucleic acid sequence from China (Wuhan-Hu1), or using antigens and antibodies derived from the virus with this sequence11. With the evolution of viral variants, any test that detects nucleic acids, antigens, or antibodies has the potential to be impacted.
Fortunately, based on available data thus far, our existing diagnostic tests perform well at detecting VOC. Some of the molecular tests that detect the RNA sequence may show a pattern of results that is different from with the original SARS-CoV-2 virus. However, this can be used to our benefit by using the pattern as a clue to learn that a variant is present12.
Therapeutics are used for the treatment of the disease. And in terms of therapeutics, studies indicate that some of the newly developed monoclonal antibodies, which block the SARS-CoV-2 spike protein and prevent the virus from attaching to cells, may be less effective against VOC. Specifically, B.1.351, P.1, and B.1.617 all show reduced susceptibility to monoclonal antibodies such as bamlanivimab and etesevimab, although they remain susceptible to other combinations of monoclonal antibodies. 7, 13 In addition, some of these VOC show decreased susceptibility to convalescent plasma, which is obtained by collecting blood from patients who have recovered from COVID-19 and infusing the antibody-rich plasma to other patients.
Vaccines: Currently our biggest pharamaceutical weapon against SARS-Co-V-2 are vaccines, which were developed in record speed via amazing feat of collaborative science. As variants emerge, the biggest concern is that these vaccines will become less effective over time. The adenoviral vector-based vaccines (produced by Astra Zeneca, Janssen, Gamaleya/Sputnik V), mRNA-based vaccines (Pfizer-BioNTech, Moderna), inactivated whole vaccines (Sinovac, Sinopharm), and protein-based vaccine (Novavax) all induce the production of antibodies to the spike protein. 14, 15 With variants, there is the possibility that the immune response elicited by vaccines, while effective against the original SARS-CoV-2 virus, may not work against an altered spike protein present on variants. Fortunately, both laboratory and clinical data thus far suggest that our vaccines remain effective against circulating VOC, especially in terms of preventing severe disease.7
Studies have suggested that the greatest potential loss of efficacy occurs against the B.1.351 variant, which was first detected in Brazil, but existing vaccines still prevent severe disease even with this variant. However, it is inevitable that with time, the virus will evolve to escape the antibodies produced by existing vaccines and we will be faced with new variants.
So, what can we do?
How do we prevent new variants from emerging?
Reducing viral transmission is the only way to prevent the emergence of new concerning variants. Why? Because mutations are a result of viral replication. Therefore, when you take precautions to limit the spread of the virus via masking, social distancing and getting the vaccine as early as you can, you are actually supporting a much larger cause, helping to save current and future lives of those in your community, country and in the world.
If you are wondering if your efforts actually matter, you will be glad to know that the science backs up your efforts. Our experience over the past year suggests that there are two main modalities for curtailing SARS-CoV-2 transmission: widespread vaccination and the observance of public health interventions such as social distancing and wearing masks. Real-world studies have shown that vaccine effectiveness at reducing SARS-CoV-2 infection, including due to VOC, can be up to 90%. 15, 17 Similarly, studies from around the world support the use of public health interventions in reducing SARS-CoV-2 transmission. 18, 19
Should we worry about airborne transmission?
The short answer is yes. A growing and compelling body of evidence suggests that the spread of the virus through touch or contact with objects is less common than spread through droplets or fine aerosol particles, which are either inhaled or land on mucous membranes such as the mouth or eyes (for example, through splashes and sprays). 20 Activities such as speaking, singing, or even breathing can all result in the dispersal of particles containing SARS-CoV-2. Case studies point to instances where many got infected in settings of indoor dining and in church settings with choirs despite social distancing. 21
Although our understanding of how SARS-CoV-2 spreads continues to evolve, the basic public health interventions that have been recommended since the beginning remain a cornerstone in battling this pandemic: physical distancing, wearings masks, adequate ventilation, avoiding crowded indoor spaces, and sanitising hands.
What are the public health policy implications?
The public health policy implications are very clear. First, is that we have to use multiple methods to combat this virus and keep new variants from emerging. Vaccination alone will not help us stay safe. Therefore, policy should guide the public towards a double layered approach: getting the vaccine as soon as it becomes available and continuing to use non-pharmaceutical methods such as masking, sanitising, physicially distancing for the foreseeable future.
Second, is that at a policy level we should be pro-active and avoid relaxing of public health measures early as vaccination coverage increase in each region. Although, extremely stringent measures such as lockdowns can be eased with a declining case-load and increasing vaccinations, a reasonable amount of public health measures such as mask mandates, suspending highly crowded events, providing personal protective equipment for those exposed often (e.g. bus drivers, conductors, cashiers, receptionists) should continue.
As the director of WHO, warned the world in his latest New York times Op-Ed we should not give into ‘vaccine euphoria.’ 22 In fact, we can use the rise in cases after New Year due to relaxing public health measures as a learning experience for policy guidance.
Third, is taking the public along with policies via communication that is frequent and clear. While we all remain hopeful that the number of cases will decrease, and more severe variants will not be detected, the threat of COVID-19 looms large and will continue to do so for a while. Therefore, government should invest and focus on explaining the science to the public often and show how policies are connected to the science. Having a single point of contact for government media releases, minimising ad-hoc statements by politicians or others, and introducing brief weekly updates with relevant experts can have a significant impact on our progress as a country when facing this pandemic.
Our way forward lies in team work, where both the public and the Government move in a direction that is backed by science, prioritising saving lives while balancing economic needs. The Government’s as well as each person’s contribution to minimising infection spread will have a significant impact on our health and the health system.
(Note from the authors: As this is an overview, we have included key references for anyone who would like to learn more. We have created a reference list relevant to this article at this link: http://bit.ly/covid-19variantslka.)
(Shashika Bandara, MSc, formerly a Policy Associate at the Center for Policy Impact in Global Health at the Duke Global Health Institute, is currently a global health policy doctoral student at McGill University.
Gayani Tillekeratne, MD MSc is an Assistant Professor in the Division of Infectious Diseases, Duke University School of Medicine, and at the Duke Global Health Institute.)