Sunday Feb 15, 2026
Sunday Feb 15, 2026
Wednesday, 31 January 2018 00:00 - - {{hitsCtrl.values.hits}}
 By Shannon Jayawardena
By Shannon Jayawardena
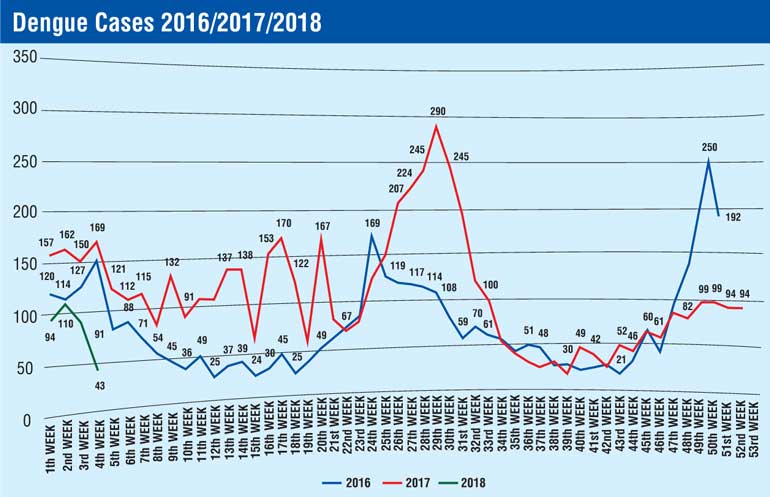
The Ministry of Health’s National Dengue Control Unit said that January 2018 had seen an overall reduction in dengue cases throughout the island, with there being 50% fewer patients compared to the same month last year.
However, areas in Jaffna, Batticaloa, Kalmunai and Puttalam have been continuing to report intermittent outbreaks as of last year, the National Dengue Control Unit observed.
According to officials from within the unit, it is important to be cautious from 6.00 to 10.00 a.m. and 4.00 p.m.-6.30 p.m. by using repellent to avoid mosquito bites. Wearing clothes that cover exposed body parts during the day and using bed nets when resting are also important precautionary measures.
While dengue is a viral infection transmitted through the bite of an infected mosquito, there are four closely related but anti-genially different serotypes of the virus that can cause dengue which are DEN 1, DEN 2, DEN 3 and DEN 4. Dengue has a wide spectrum of infection outcomes (asymptomatic to symptomatic). Hence symptomatic illness can vary from undifferentiated fever (viral syndrome), dengue fever (DF), dengue haemorrhagic fever (DHF) and dengue with unusual manifestations.
Severe vomiting, abdominal pain, increased thirst, drowsiness and excessive sleepiness, loss of appetite, abnormal bleeding manifestations, cold and clammy skin, restlessness and irritability, skin mottling, decreased or no urine output and behaviour changes such as confusion or use of foul language are the main symptoms and if present should seek immediate medical attention. It is also important to know that any acute fever with both headache and pain around the eyes, muscle or joint pain, diffused reddish rash, nausea and vomiting or any bleeding manifestation from the gum, nasal and skin are signs of a possible dengue infection.
However, early identification and management of dengue can help reduce morbidity and mortality. At the present hyper-endemic setting in Sri Lanka, dengue is considered in the differential diagnosis of patients presenting the acute onset of fever with headache, retro-orbital pain, myalgia, arthralgia, rash (diffuse, erythematous, macular), haemorrhagic manifestation, Leukopenia (<5000/mm3), platelet count ≤150,000/mm3 and rising Hematocrit of 5-10%.
If the above symptoms are observed one should seek proper early medical advice, take physical rest by avoiding any form of exercise or sport, drink adequate amounts of liquids, avoid self-medication with drugs other than the correct dosage of Paracetamol for fever, do a full blood count by day three of the fever based on medical advice and avoid non-steroidal anti-inflammatory drugs such as Ibuprofen, Diclofenac sodium, Mefenamic acid and steroids such as Prednisolone or Dexamethasone for the febrile illness.
World Health Organisation statistics state that approximately 55% of the global population who live in endemic countries in the tropics and subtropics are at the highest risk of contracting dengue while over 1.3 billion of them come from the South Asian region.
Sri Lanka suffered greatly with the substantial increase of dengue transmission during May-July last year. Numbers from the National Dengue Prevention Unit show that 185,688 dengue patients were reported in 2017 while around 400 died of the disease.
Nevertheless, immediate preventive action by Health Department officials with multi-sectorial collaboration as provided by the Presidential Task Force on dengue control curtailed the situation successfully.
Intensified disease surveillance, improvement of clinical management facilities including laboratory services, enhanced patient awareness, expanded mosquito control activities as well as the deployment of additional manpower to help the affected areas during last year’s outbreak have really contributed towards this year’s 50% reduction.