Friday Feb 27, 2026
Friday Feb 27, 2026
Wednesday, 27 February 2019 00:58 - - {{hitsCtrl.values.hits}}

By Fathima Riznaz Hafi
The statistics for women’s cancers are relatively standard around the world; while the most common cancer in women is breast cancer, gynaecological cancers, though lower in incidences, pose a significant threat, with deadly consequences if not detected and treated early.
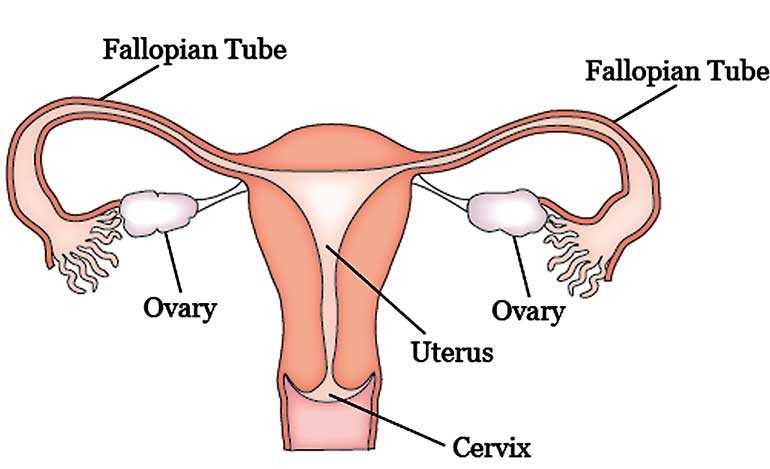
Parkway Cancer Care (PCC) Singapore Senior Consultant Oncologist Dr. Wong Chiung Ing shared that gynaecological cancers, which refer to cancers that affect the woman’s reproductive organs (ovary, uterus, cervix, etc.), account for about 30% of all women’s cancers in Sri Lanka. There is also a rare one called ‘primary peritoneal cancer’ (the peritoneum is the layer that covers these organs).
BRCA mutation
As with other cancers, there is no single cause for gynaecological cancers. “Some people are at increased risk of developing breast and ovarian cancer and this group of people have a mutation called ‘BRCA’ (the mutation that Angelina Jolie has), which is inherited from parents.
By the age of 40 or 50, the chance of developing breast cancer in the BRCA mutation carrier is up to 60%, whereas in the normal population maybe about 10-20% at most. And the chance of developing ovarian cancer is also much higher (about 30-40%),” Dr. Wong said.
“If many of your family members have a lot of cancers – breast, ovarian, pancreas, prostate – these are all somewhat related to BRCA mutation; then the risk of developing breast and ovarian cancer is much higher. If you suspect this mutation runs in the family, you have to check it – through a blood test,” she said and asserted that there are some new medicines that target against this mutation and there are things that can be done to treat the cancer.
HPV
Dr. Wong further mentioned that there is also a virus that can lead to cancer in women. “Human Papillomavirus (HPV) is a high-risk virus that can cause cervical cancer. There may be about 150 types of that, out of which about 50 can cause cancer; and it causes about 70-80% of all cervical cancers,” she said.
“The HPV test checks whether you have this virus in the cervix. HPV 16 and 18 are the commonest culprits so when we do the HPV test we usually test for these two; we also test for others depending on the case but these two definitely need to be tested.”
As it is a virus, vaccines have been developed for protection, as is done for other viruses such as the flu. “It’s the same principle; you give the vaccine – the deactivated virus – keep it inside and hope that the body will create some sort of antibody against this virus; so when the real thing comes, they know how to attack it – that’s the principle of vaccination,” Dr. Wong explained.
“In Singapore, we vaccinate girls as young as nine years old (we want to protect them ‘before’ they have sex) and it’s given three times: day one, one month later and six months later – it’s almost like the Hepatitis vaccine. This is to prevent girls from getting cervical cancer.” Asked if it’s for all girls or only girls who are at risk – such as if they have it in the family, she replied, “It’s for all girls; because the risk is sex – HPV is transmitted by sex so we need to vaccinate before they are sexually active.”
“But even though we vaccinate them, it doesn’t guarantee that they won’t get cervical cancer – that’s a misconception! You still need to get your Pap smears, etc. done, as soon as you have sexual activity,” she cautioned.
Symptoms
The symptoms vary for different gynaecological cancers. Though the organs are from the same region in the body, each one is treated somewhat differently because they present differently. But the commonest symptom or presentation is usually abnormal vaginal bleeding.
Any abnormal bleeding, such as inter-menstrual bleeding, bleeding after sex, painful intercourse or post-menopausal bleeding, are the commonest presentation of gynaecological cancers, she said. And because gynaecological organs are very near the bladder and rectum, some people may present with difficulty passing urine or motion.
“Symptoms for cervical cancer and uterus cancer are somewhat similar – usually it’s abnormal vaginal bleeding. And cervical cancers are very advanced – they can spread left, right, up, down, centre; so sometimes they may block the bladder – the person will have problems passing urine, they will block the bowels – so you have problem passing motion; because this is in between our bladder and rectum. And they block not only the bladder but also the kidney because the bladder connects up to the kidney and the kidney may become swollen and you can get back pain from that.
“For ovary cancer, the early stages, usually are not very symptomatic – which is very sad because ovarian cancer patients present quite late, usually at stage 3 and when that happens they may have big masses in the ovary; and they may have some involvement of the peritoneum – a layer that covers the intestine, ovaries, etc. and when that happens they can get swelling and bloating, loss of appetite and lethargy,” she said.
Diagnosis, treatment and new advances
“For diagnosis, first we will be guided by symptoms and second we need to examine either with an ultrasound or a biopsy – and if the diagnosis is confirmed, we need to do a pet scan to see whether the disease has spread.
The treatment for each one is a bit different; ovarian cancer is usually treated by surgery, followed by chemotherapy, depending on the stage. For uterine cancer, usually surgery is done first, followed by either chemotherapy or sometimes radiotherapy. Treatment for cervical cancer depends on the stage – at the early stage it is treated with surgery, while at the advanced stage the treatment is with surgery and chemotherapy. The earlier the diagnosis the higher the chance of survival.
“There have been new advances in treatment; in general the backbone of treatment is surgery, chemotherapy and radiotherapy; but we now have some new developments in the treatment of gynaecological cancers. We know that the cells need blood supply to grow and to have food; so there is a drug that we can use to cut off the blood supply to the cancer cells. This drug is called ‘Avastin’ and can be used in all kinds of gynaecological cancers in combination with chemotherapy.”
“One of the other advances is immunotherapy but it is still being evaluated; not the standard of care yet and if we want to give it we have to check for certain expression on the tumour itself before we give it because it’s very expensive.”
Immunotherapy works again through infusion and goes into the body – it will stimulate the immune system to fight the cancer. It’s a new treatment option and is being used for a lot of cancers; its use is established in some cancers such as melanoma, lung cancer, kidney cancer; but in breast and gynaecological cancers it is not used unless checked to see whether the patient is suitable for it.
Screening
Dr. Wong wrapped up by emphasising the importance of screening. “As an oncologist, it’s very sad that we always see patients coming with cancer; if you can screen and detect it early it could save you.”
In Singapore, the screening program is such that after a woman turns 40 years old she does a mammogram every year until she is 50 years old; and then if that’s normal she does it every two years until she is 70 years old. For gynaecological cancers – ovarian and uterus – they don’t have many screening programs but for cervix there is a one – they usually start at 25 years old especially if they have had sex, and they do it every year, and every year if it’s normal they can do a Pap smear every three years, she said.
Dr. Wong stressed that early screening is crucial and loss of lives can be easily prevented if we take the necessary steps to get tested before it’s too late.