Friday Feb 27, 2026
Friday Feb 27, 2026
Wednesday, 19 December 2018 00:00 - - {{hitsCtrl.values.hits}}
The only way that we will actually bring health care to every person, everywhere in the world, is if we fundamentally change the system so that governments and people demand more investments in health – World Bank Group President Jim Yong Kim
When Cecilia Rodriguez was diagnosed with rheumatoid arthritis, an autoimmune disease that causes inflammation and pain in the joints, eight years ago, she had a major revelation. She realised that what she was promoting as director of a primary health care facility in Chile was very different than what she actually needed as a patient.
In response, she founded the nonprofit Fundación Me Muevo with her sister, who also has rheumatoid arthritis, to support people affected by the chronic condition. She also became a patient advocate – Me Muevo is part of a growing movement of patient-led organisations in Chile.
“Health care systems tend to be geared towards treating acute illnesses and are rarely organised to help patients with lifelong diseases,” Cecilia says. “We called the NGO Me Muevo (‘I move’) because we learned that with this condition you have to keep your body moving, but also because ‘I move’ means ‘I take action.’”
Cecilia is part of a large and growing global movement working to ensure that universal health coverage (UHC) becomes a reality. UHC is based on the simple idea that all people should be able to access the quality health services they need, without suffering financial hardship.
Health for all by 2030
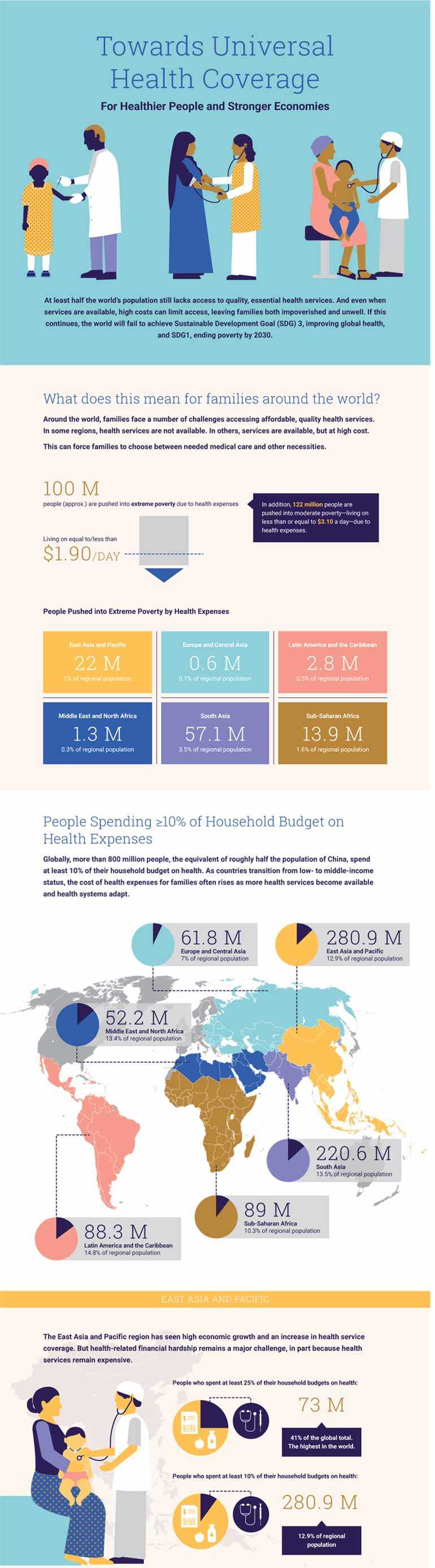
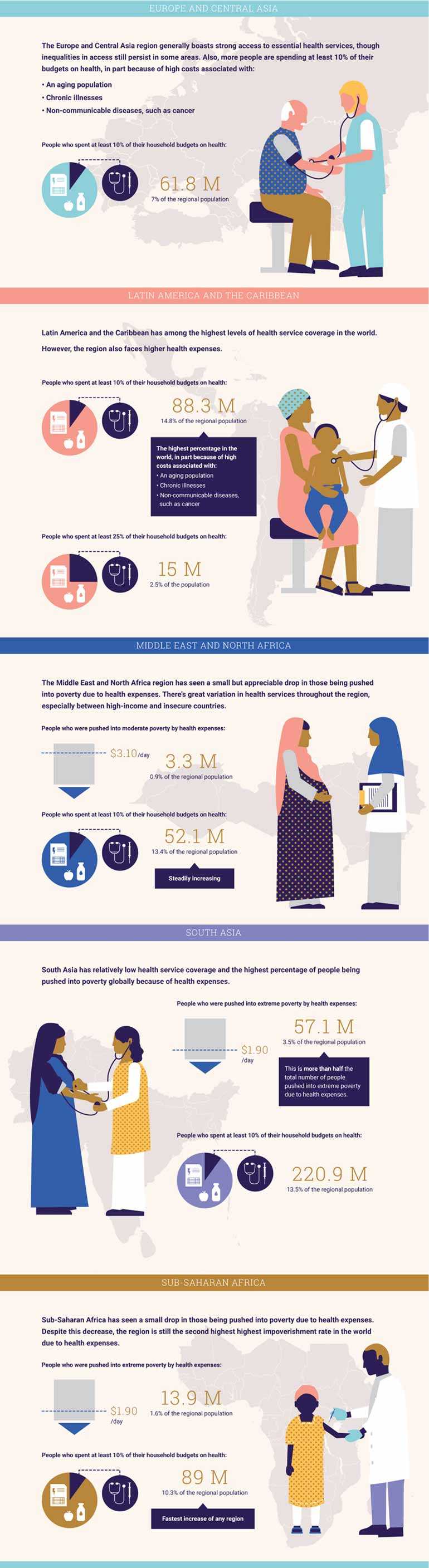
UHC Day, celebrated on 12 December every year, is a time to highlight the worldwide progress towards UHC. Thanks to strong national leadership and ambitious reforms, most parts of the world have seen an expansion in access to health services and action to ensure affordability. However, despite this, according to recent research from the World Bank Group and World Health Organization (WHO).
Attaining UHC by 2030 is a global commitment under the Sustainable Development Goals. It is also key to meeting the Bank Group’s twin goals of ending extreme poverty and increasing shared prosperity – these cannot be realised as long as millions are being impoverished by health expenses every year. Providing affordable, high quality services is a challenge for countries at all income levels, as data from 183 countries in the Bank Group’s 2018 Health Equity and Financial Protection Indicators (HEFPI) database indicates.
The cost of health care is a major financial burden on families. Around the world 800 million people spend at least 10 percent of their household budgets to pay for health care, often forcing them to choose between their health and other necessities for their family, such as food, school fees or transportation. If these 800 million people lived in one country, they would make up the third biggest population in the world. This financial burden is seen in all regions of the world.
Such large numbers can obscure the daily suffering individuals and families face when they can’t get the health care they need: the infant who isn’t immunised and dies from pneumonia; the stunted child whose school performance and learning is permanently impaired; the pregnant teenager who can’t secure family planning services and is forced to drop out of school; and the mother who is hemorrhaging post-partum without access to blood transfusions.
Lack of health care is a waste of human capital
This denial of health care is not only unjust, it is also a waste of human potential and a country’s human capital. Human capital is the knowledge, skills and health that people accumulate over their lives, enabling them to realise their potential as productive members of society.
Health is a foundational element of a country’s human capital. Without good health, children cannot go to school and learn, and adults cannot work and contribute to their households and economies. A healthy, educated and resilient population is a must for countries to compete effectively in the global economy.
“The only way that we will actually bring health care to every person, everywhere in the world, is if we fundamentally change the system so that governments and people demand more investments in health,” says World Bank Group President Jim Yong Kim.
When investments in health begin in the early years of life and are sustained through the life cycle--for infants, children, adolescents, adults and seniors – they lay a strong foundation for the growth and competitiveness of nations. Each additional healthy year of life should be thought of as the fuel that makes economies grow, which is why UHC means investing across the life-course.
The path to UHC is different for each country, and the World Bank Group supports countries by providing financing, policy advice and technical assistance, generating research and knowledge and convening a range of stakeholders around shared goals. UHC is the driving force behind the Bank Group’s health, nutrition and population investments, which in FY18 totaled about $14 billion.
Through its new Human Capital Project, an effort to accelerate more and better investments in people, the World Bank Group has committed to scaling up its investments in areas like health. The project’s Human Capital Index measures and ranks countries according to the amount of human capital a child born today can expect to attain by age 18 through investments in health and education—and shows how much income countries are foregoing because of human capital gaps. Country governments are the greatest drivers of change and investment in human capital, including health.
Accelerating progress: 5 ways to get there
There’s no magic bullet or single path to achieving UHC by 2030, but here are five essential elements for accelerating progress:
More money for health, and more health for the money
The health sector faces a severe crisis of underinvestment. The cost of essential health services globally is put at about $90 per person per year. In 2015, 71 countries invested less than this in the health of their citizens, and 41 nations, with a combined population of 2.6 billion, invested less than $25 per person. Countries also need to improve the efficiency of their investments in the health sector, to ensure they are getting the best possible outcomes. External development assistance for health and other global partnerships can play a complementary and catalytic role to domestic resources, which form the vast majority of investments in health at the country level.
Focusing on quality of care
Access and affordability of health services alone are not enough – health care also needs to be of high quality. Three recent global reports, including a joint report from the World Bank Group, the WHO and the Organization for Economic Co-operation and Development (OECD), make clear that poor quality health services are holding back progress on improving health in countries at all income levels. For example, 10% of hospitalised patients in low and middle-income countries can expect to acquire an infection during their stay, and seven percent in high-income countries. There has been some progress in improving quality though, for example in survival rates for cancer and cardiovascular disease.
Protecting all people from pandemics
There’s been a steady increase in the frequency and diversity of disease outbreaks over the past 30 years. Epidemics can strike anywhere. But it’s often the weakest part of the health system, where people are not being reached by health services, is often where outbreaks grow unchecked. We can all be protected from outbreaks and pandemics only if every single person is covered by health services—which is the foundation of UHC. This is why the World Bank Group focuses on supporting countries strengthen veterinary and human health systems through its Regional Disease Surveillance Systems Enhancement (REDISSE) program, and has pioneered innovative financing of speedy response to pandemics through the Pandemic Emergency Financing Facility (PEF).
Embracing innovation
UHC by 2030 cannot be achieved by a “business as usual” approach. Countries that have been successful have embraced innovation in a way that can transform health systems. The WBG report Business Unusual looked at how countries have bent the curve of progress. Rwanda has used an innovative private sector partnership, for example, to cut the delivery time for life-saving blood by using drones. Afghanistan has seen sharp improvements in maternal and child survival health and nutrition despite insecurity by contracting with local NGOs to provide basic health services. Innovative financing approaches helped shape the Turkish government’s transformation of its health care sector while the Global Financing Facility (GFF), a country-led innovative financing platform, is now active in 27 countries catalysing large scale investments in women and children’s health and nutrition.
Mobilising for collective action
Making UHC by 2030 a reality requires empowering people, communities and civil society to be full and active participants in the UHC movement, to hold governments accountable for ensuring high quality, affordable and accessible health care. People should be aware of what they are entitled to from their health system, involved in designing health care that responds to their needs, and engaged in monitoring health care so that they can advocate for change when it doesn’t deliver what it promises. UHC2030, a global movement of institutions, governments and CSOs to build stronger health systems for UHC, is co-convened by the WBG and the WHO to ensure this.
There is political commitment and country leadership like never before-- but global progress must be accelerated to ensure UHC by 2030. It will take effective leadership, the right policies and investments and an overarching commitment to “put the last mile first” and reach the most vulnerable. There is no time to waste.
(Source: http://www.worldbank.org/en/news/immersive-story/2018/12/07/lack-of-health-care-is-a-waste-of-human-capital-5-ways-to-achieve-universal-health-coverage-by-2030?cid=ECR_E_NewsletterWeekly_EN_EXT&deliveryName=DM7442)